Blog
Build vs. Partner: A Strategic Guide to Scaling Commercial Insurance for Virtual Care
Speed, scale, or control? A decision-making guide for virtual care leaders navigating commercial insurance expansion.

Executive Summary
For digital health companies aiming to scale nationally with insurance coverage, a critical decision looms: should you build the infrastructure internally or partner with an external platform?
While internal buildouts may seem appealing from a control and cost-ownership standpoint, the operational burden, regulatory risk, and extended timelines often undermine strategic momentum. This paper outlines the full scope of what it takes to stand up national insurance operations internally — across contracting, compliance, credentialing, billing, and technology — and compares that to what a proven partner can unlock.
Our analysis shows that for most virtual care startups, internal builds require 2-3 years to get to national coverage, cross-functional investments across 8–10 teams, and a dedicated budget of several million dollars. In contrast, an experienced infrastructure partner can reduce this to under 60 days, with materially lower risk and cost.
The Full Scope of Building Insurance Infrastructure In-House
Scaling insurance operations isn’t a matter of securing a few payer contracts. It involves building a complex, multi-layered system that spans contracting, clinical workflows, compliance oversight, and technical integrations.
Here’s a breakdown of the major workstreams required to do this internally:
Health Plan Strategy & Contracting
Market Mapping: Identify key national and regional payers per state and per specialty.
Contract Negotiations: Requires multiple rounds of discussions with legal, network management, and clinical teams on the payer side.
Meeting requirements: Many health plans require provider groups to hold a Medicare and/or Medicaid contract in the state, have clinicians that live in the state, and have hospital admitting privileges.
Rates: Depending on maturity, size, and clinical specialty, rates can vary significantly. Rate negotiations require detailed analytical justification and substantial volume.
Timelines: 6–12 months to secure multi-state contracts (longer if starting from scratch).
Team Required: General Counsel, Head of Payer Strategy, Clinical Director.
Clinical & Legal Compliance
Clinical Infrastructure: PC setup in 50 states, providers licensed in each state.
Policy Development: SOPs for documentation, patient consent, assignment of benefits, prescribing, coverage limits by plan/state.
Licensure Audits: Ensure provider licensure and scope of practice compliance across 50 states.
Audit Preparedness: Build documentation and workflows to support payer audits.
Team Required: Medical Director, Legal & Compliance, Clinical Ops.
Credentialing & Enrollment
Credentialing processes: All providers should go through a formal internal credentialing process. Alignment to NCQA standards is best practice.
CAQH Management: Each provider must have an updated CAQH profile, re-attested every 120 days.
Payer-Specific Enrollment: Each plan requires a unique credentialing and enrollment process. Plan to complete one enrollment per provider per state — so one provider with 15 state license will result in 45-60 enrollments into the major health plans.
Integration into scheduling: Provider licensure and plan enrollment information must integrate with scheduling systems to match patients with providers who are both licensed in the patient's state and enrolled with their insurance plan.
Timeline: 60–120 days per provider, per payer.
Team Required: Credentialing Manager, Operations Analyst, Provider Support.
Revenue Cycle Management (RCM)
Billing Infrastructure: Select a billing software (e.g. Candid Health), hire or contract an RCM team, build integration between EMR and billing software.
Eligibility Checks: Implement real-time and batch eligibility workflows, or standup manual eligibility check process with back-office team.
Denials Management: Staff trained to resolve rejections and appeals.
Patient Collections: Ensure compliant, friendly payment collection processes.
Team Required: RCM Lead, Medical Coder, Claims Processor, Billing Software Engineer.
Technology Infrastructure
API Integrations: Connect EMR, scheduling, and intake flows with billing systems. Setup a real-time benefits verification system.
Data Security: Ensure HIPAA compliance from Day 1.
Reporting Dashboards: Real-time visibility into claims, denials, reimbursements.
Team Required: EMR Integrations Engineer, Security & DevOps, Data Analyst.
Estimated Timeline & Cost of Internal Build
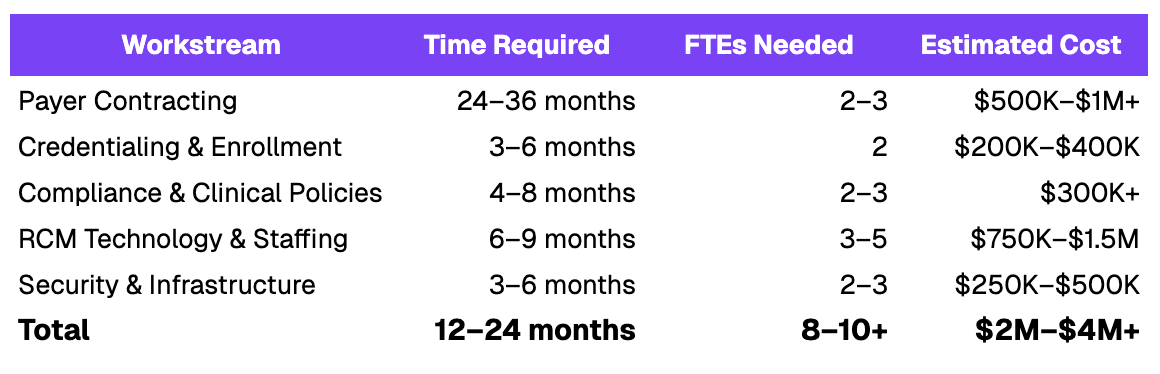
Note: Costs exclude ongoing operational headcount and overhead required to maintain the system post-launch.
Strategic Risks of the Internal Build Path
Time to Market Risk: Delays in contracting or enrollment can cost months of revenue and momentum, especially if payer negotiations stall.
Operational Complexity: Insurance operations are non-core to most digital health teams. Spreading attention across clinical, tech, compliance, and billing weakens focus.
Credentialing Bottlenecks: Provider onboarding can become a growth limiter if your credentialing and enrollment workflows aren’t scalable from Day 1.
Compliance Exposure: A misstep in billing compliance or documentation can trigger audits, clawbacks, or provider de-enrollment.
Missed Revenue: Inaccurate eligibility checks or inaccurate-coding leads to denied or underpaid claims -- often unnoticed for months.
The Case for Partnering
By partnering with a purpose-built infrastructure provider, companies can:
- Go Live nationally in weeks, not quarters: Fast-track national payer access and start billing within weeks.
- Reduce Engineering & Ops Burden: Offload credentialing, compliance, and RCM to a specialized team with scalable systems.
- Drive Faster Revenue Ramp: Our partners have scaled to thousands of monthly insurance-covered visits within 3–6 months of launch.
- Ensure Audit-Ready Compliance: Built-in SOPs, documentation standards, and real-time eligibility reduce risk of denials and penalties.
Conclusion
For most digital health companies, time, focus, and execution risk are the biggest barriers to building insurance infrastructure in-house. Unless insurance is your core competency, the case to partner is overwhelmingly strong, especially if speed to market and scalability are strategic priorities.
If you're evaluating the build vs. partner decision, we’d be happy to share benchmarks, timelines, and case studies to guide your thinking.
.png)